“Exploring ‘The Menopause Brain’ with Neuroscientist Dr. Lisa Mosconi at Washington Post Live

Greetings, and a warm welcome to Washington Post Live. I’m Tara Parker-Pope, serving as the editor of the Well+Being desk at The Post.Today, I’m thrilled to be in conversation with Dr. Lisa Mosconi, a distinguished neuroscientist and best-selling author of the recent publication, “The Menopause Brain.” Dr. Mosconi, I appreciate your presence at Washington Post Live.
READ: Navigating Amsterdam’s Waterways: A Canal Cruise Experience
The Menopause Brain
MS. PARKER-POPE: Delighted to have you. The topic you’re addressing is profoundly significant, impacting countless individuals. To commence, could you share what motivated you to pen this book? With numerous books on menopause already available, what led you to believe there was a need for “The Menopause Brain”?
DR. MOSCONI: There were several factors inspiring the creation of this book. My ongoing research as a neuroscientist, heading the Alzheimer’s prevention program at Weill Cornell Medicine in New York City, contributed significantly. We actively investigate the menopause brain, examining the associated risks and vulnerabilities. Additionally, numerous women reached out to me, sharing their experiences of cognitive, emotional, and psychological symptoms during menopause, including the often-overlooked symptom of brain fog, causing legitimate concerns about early onset dementia. Bridging the gap between research in the lab and accessibility for all women motivated me to write a book. I believe it can reach a broader audience than I can directly engage with in my research.
MS. PARKER-POPE: How do you define the menopause brain, and how does it differ from the teenage or younger woman’s brain?
DR. MOSCONI: The menopause brain is characterized by a state of transition, a significant change occurring as part of the neuroendocrine transition of menopause. This transition impacts the neurological and hormonal systems simultaneously, leading to a rewiring and remodeling within the brain. While this change is biologically essential, it also introduces vulnerabilities, manifesting as symptoms like hot flashes, night sweats, insomnia, anxiety, depression, mood swings, and notably, brain fog and memory lapses.
Interestingly, when examining the brain itself, the changes experienced during menopause aren’t vastly different from those during puberty or pregnancy. The menopause brain can be viewed as an extension of the changes observed during crucial turning points in a woman’s life. These transitions trigger brain remodeling, offering both vulnerabilities and increased emotional strength, a facet often overlooked in societal discourse.
MS. PARKER-POPE: The foreword of your book, written by Maria Shriver, underscores the challenges women face during menopause, describing it as a “function of the brain that plays havoc with a woman’s body and her outlook on life.” The first chapter is titled “You Are Not Crazy.” Could you elaborate on why it has been challenging for both women and the medical community to acknowledge the normalcy of menopause and dispel the notion of women being perceived as “crazy” due to these real symptoms?
DR. MOSCONI: The historical perspective on menopause, traced back to Darwin, initially characterized it as a phase nature had not intended. Darwin, a key figure in modern biology, held biased views on women’s brains, suggesting inherent inferiority. This perspective influenced medical and scientific narratives for a prolonged period. Research was predominantly conducted on men or male animals, aiming to validate Darwin’s belief in the superiority of men’s brains. This led to a form of “bikini medicine,” where only body parts fitting under a bikini line were considered essential to defining women. The focus on women’s brains was minimal, as they were deemed equivalent to men’s brains—merely smaller, more complex, and prone to hormonal fluctuations, making them seemingly unworthy of study.
This ageist and sexist attitude, combined with a cultural bias against menopause, has contributed to emphasizing the downsides rather than recognizing menopause as a potentially helpful evolutionary phase for women.
MS. PARKER-POPE: Approximately three-quarters of women experience brain symptoms during menopause, as mentioned in your book. Could you delve into what these symptoms entail?
DR. MOSCONI: Certainly. Brain symptoms during menopause encompass a range of experiences. The most prevalent symptom is hot flashes, often misunderstood as skin or temperature-related issues. In reality, hot flashes are neurological symptoms resulting from menopause-induced changes in a specific brain region, the hypothalamus, responsible for regulating body temperature. Over 75% of women encounter hot flashes during the menopausal transition.
Mood changes, sleep disturbances, including insomnia, and brain fog with memory lapses are also common. More than 50% of perimenopausal and postmenopausal women report experiencing sleep disturbances. These symptoms collectively contribute to the challenging menopausal experience.
MS. PARKER-POPE: During our Women’s Health Summit, you presented fascinating brain scans comparing a woman’s brain before and after menopause. Could you offer insights into what these scans reveal?
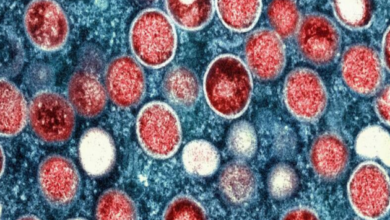
DR. MOSCONI: Absolutely. These scans, conducted using positron emission tomography (PET) scans with a tracer called fluorodeoxyglucose, depict brain energy levels. The scans compare a woman’s brain before menopause and approximately eight years after the transition.
In the “before” scan, bright red and yellow colors represent high brain energy levels, creating an image of a vibrant and active brain. The green shades indicate lower energy levels. After menopause, the colors shift, with red turning to yellow and yellow to green, reflecting a 30% reduction in brain energy levels. This reduction signifies the significant changes occurring in the menopause brain.