Exploring the Potential of Suvorexant to Mitigate Opioid Addiction while Preserving Analgesic Effects
Heroin use disorder and chronic opioid administration are significant public health concerns, affecting millions of individuals worldwide. Chronic opioid use, whether in humans or animal models like mice, leads to substantial alterations in the brain’s hypocretin (Hcrt, or orexin) system, which plays a crucial role in regulating wakefulness, arousal, and reward. Understanding these changes is vital for developing strategies to mitigate the adverse effects of opioid use while preserving their analgesic benefits.
READ: Navigating Amsterdam’s Waterways: A Canal Cruise Experience
Impact of Chronic Opioid Use on Hypocretin Neurons
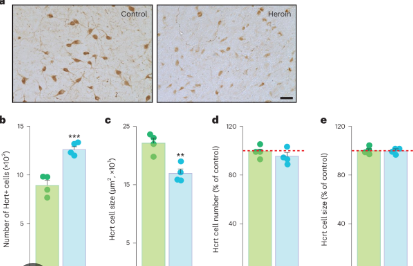
Research has demonstrated that heroin use disorder in humans and chronic opioid administration to mice result in an increase in the number of detected hypocretin neurons and a decrease in their size. Hypocretin neurons, located in the hypothalamus, are integral to maintaining arousal and regulating the body’s reward system. These changes suggest a significant restructuring of the hypocretin system in response to prolonged opioid exposure.
In animal studies, chronic morphine administration leads to increased Hcrt axonal projections to the ventral tegmental area (VTA), a critical region in the brain’s reward circuitry. This increase is accompanied by elevated levels of tyrosine hydroxylase (TH), an enzyme essential for dopamine synthesis, and a higher number of TH+ cells in the VTA. Additionally, chronic morphine activates microglia, the brain’s immune cells, in both the VTA and the hypothalamus. These findings indicate that chronic opioid use induces widespread changes in brain regions involved in reward and addiction.
The Role of Suvorexant in Modulating Opioid Effects
Suvorexant, a dual hypocretin receptor antagonist commonly used for treating insomnia, has shown promise in modulating the effects of opioids. When co-administered with morphine, suvorexant prevents several morphine-induced changes. It halts the increase in the number of hypocretin neurons, preserves their size, and prevents the augmentation of Hcrt projections to the VTA. Additionally, suvorexant inhibits microglial activation in the VTA and hypothalamus.
One of the most significant findings is that suvorexant, when combined with morphine, prevents morphine anticipatory behavior, a hallmark of addiction, and reduces opioid withdrawal symptoms. These results suggest that suvorexant can mitigate some of the adverse behavioral effects associated with chronic opioid use.
Maintaining Analgesic Effects
Crucially, while suvorexant alters the brain’s response to morphine, it does not diminish morphine’s analgesic effects. This is a significant finding because it suggests that suvorexant can be used to reduce the addiction potential of opioids without compromising their pain-relieving properties. Chronic pain management often necessitates long-term opioid use, and the risk of addiction is a significant concern. The ability to maintain analgesia while reducing addiction risk is a major advancement in pain management strategies.
Implications for Human Health
The findings from these animal studies have profound implications for human health. Opioid addiction remains a significant challenge, with millions struggling with dependency and the associated health risks. The potential to use suvorexant as an adjunct therapy with opioids offers a promising avenue for reducing the risk of addiction.
Furthermore, the preservation of analgesic effects means that patients with chronic pain conditions could potentially receive effective pain relief without the heightened risk of developing an opioid use disorder. This dual benefit addresses two critical concerns in pain management: effective analgesia and reduced addiction risk.
Conclusion
The combination of opioids with suvorexant represents a promising strategy for managing pain while mitigating the risks of opioid addiction. By preventing opioid-induced changes in hypocretin neurons and microglial activation, suvorexant not only reduces addiction-related behaviors but also preserves the analgesic efficacy of opioids. These findings highlight the potential of suvorexant to transform pain management practices and offer new hope for individuals struggling with chronic pain and opioid addiction. Further research and clinical trials will be crucial in translating these findings into practical treatment protocols, potentially providing a safer and more effective approach to pain management in the future.